Introduction:
Due to the graft versus tumor effect allogeneic stem cell transplantation (allo-SCT) is a curative strategy for hematological malignancies. However, its benefits are offset by non-related mortality (NRM) primarily from graft-versus-host-disease (GVHD). In vivo T-cell depletion (TCD) with Anti-T-Lymphocyte globulin (ATLG) can reduce GVHD. Although lower ATLG doses may compromise the immunosuppression effects, higher ATLG doses may offset its benefit by decreasing antiviral and graft-versus-malignancy effect by depletion of donor effector T cells. Even though the use of ATLG in allo-SCT is well established, however, data on optimal ATLG dosing in the setting of matched sibling donor (MSD) -allo-SCT is scarce.
Methods:
In this retrospective study conducted at the Department of stem cell transplantation, University Medical Center Hamburg Eppendorf (UKE) we aim to compare the transplant outcomes between recipients of 15 mg/Kg vs 30 mg/Kg ATLG as T-cell depletion in Patients undergoing allo-SCT from MRD.
Results:
In the study, 109 sequential patients (ATLG 15, n=72; ATLG 30, n=37) underwent allo-SCT between the years 2018 and 2022 from MSD for hematological conditions. PBSC was the primary stem cell source in both cohorts (ATLG-15, 99%; ATLG-30, 92%; p=0.08). In the ATLG-15 group, 13% received TBI versus none in the ATLG-30 group (p=0.025). The MAC regimen was utilized in 65% of ATLG-15 patients, compared to 27% in ATLG-30 (p<0.001). The most prevalent disease was AML in ATLG-15 (54%) and PMF in ATLG-30 (54%, p<0.001). More ATLG-15 patients were transplanted in CR (43%) than in ATLG-30 (16%, p=0.02). All ATLG-15 patients had ECOG0-1 status, against 90% in ATLG-30 (p=0.007). The median age at transplant was similar, 58 and 56 years in ATLG-15 and ATLG-30, respectively (p=0.99). All other Patients donor and transplant characteristics were comparable between the two groups.
One patient died prior to engraftment and three patients had primary graft failure in the ATLG-15 group, all remaining patients successfully engrafted. The ATLG-15 cohort showed an earlier leukocyte engraftment (median 11 days, range 9-19, p=0.001) and a tendency towards quicker platelet engraftment (median 12 days, range 8-107, p=0.06) compared to the other group's medians of 13 days (range 8-16) and 17 days (range 3-130), respectively.
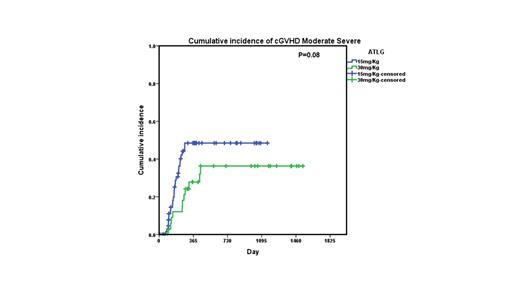
Grade II-IV aGVHD at day 100 was 36% in the ATLG-15 group compared to 23% in the ATLG-30 group (p=0.45). A trend towards lower 2-year moderate/severe cGVHD was observed in the ATLG-15 group (48% vs 36%, p=0.08).
The ATLG-15 group showed a trend towards higher 2-year OS (84% vs 72%, p=0.06), however this trend disappeared on multivariate analysis (MVA) (HR 0.853 [95%CI 0.319, 2.283]; p=0.75) no other factor affected OS on MVA. The 2-year PFS was similar across both groups (ATLG-15, 63%; ATLG-30, 60%; p=0.5). On MVA only TBI had a significant effect on PFS (HR 0.310 [95%CI, 0.101, 0.957], p=0.04), none of the other factors significantly affected PFS.
There was a trend for Lower NRM in the ATLG-30 group (at 1 Yr, 0% vs 11%, p=0.09), while the two-year relapse incidences were comparable (ATLG-15, 7%; ATLG-30, 14%; p=0.2).
Conclusion:
Acknowledging the retrospective nature of our study, however our results show that a higher ATLG dose may reduce incidence of chronic GVHD in Patients undergoing allo-SCT from MSD, however our findings should be confirmed in larger prospective studies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal